I’ve visited hundreds of healthcare facilities over the years, as architect, owner’s representative, facility operator and product representative. This last month I visited the University of California Irvine (UCI) as a patient. This turned into a journey in resolving a congenital heart condition that I didn’t even know I had… and impacts 27% of the population.
Read more for my unique, humbling in-person “Patient Experience”


(Full disclosure – I am a retired hospital architect from another UC Health location, currently working on biomedical research facilities, improving healthcare environment performance and reducing infections).
Background
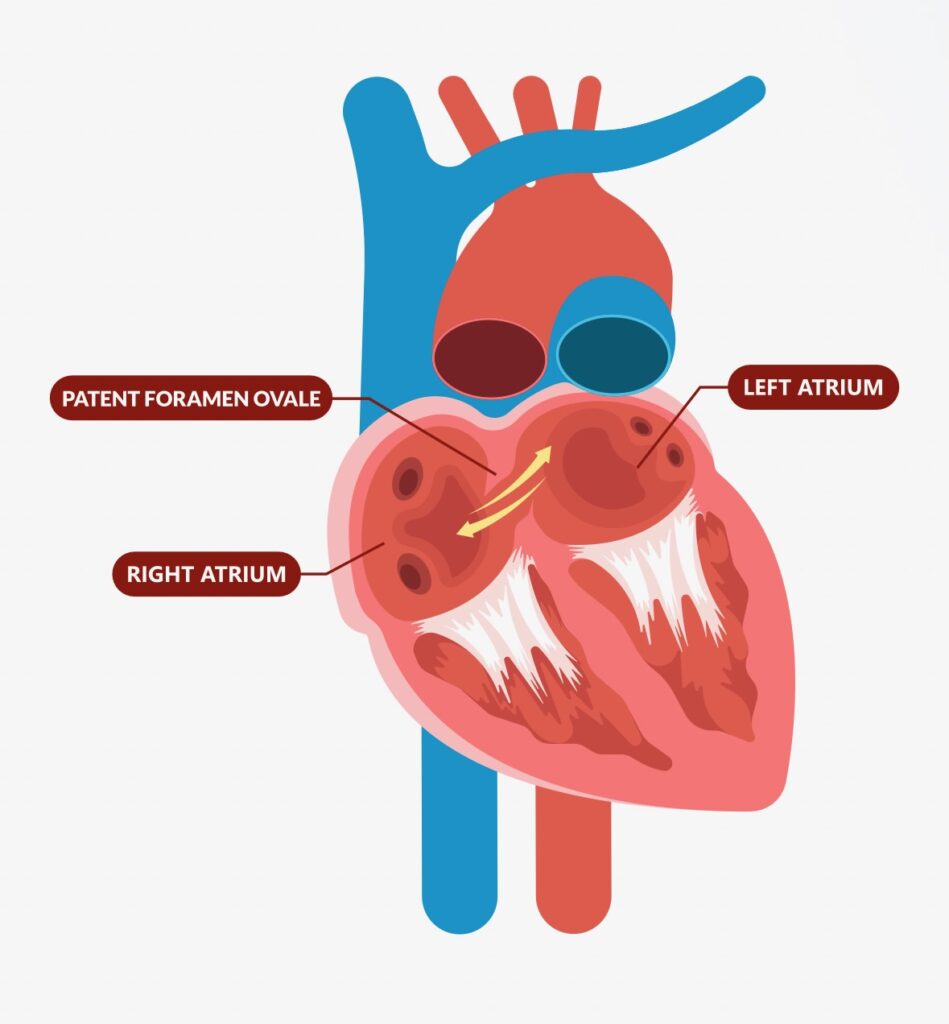
Without getting into the weeds too much, I found myself at Disneyland in March 2025. Instead of visiting Mickey and Co, I suddenly was in need of the hospital. I thought I recognized the pain as kidneystones and knew I needed to get care. University of California Irvine’s emergency room in Orange was only a few miles from Disneyland, so I popped in for a quick treatment. Little did I know that this would lead to a week of tests and procedures to determine the real cause of my issues. The answer: a congenital hole between the left and right atria called a Patent Foramen Ovale (PFO). The Cleveland Clinic defines the PFO as a small hole between the upper chambers of your heart that may let blood clots travel to your brain or other organs. In short, closure reduces the potential of a much worse conditions such as a stroke. So glad to find this from a pain in my kidney instead!
https://my.clevelandclinic.org/health/diseases/17326-patent-foramen-ovale-pfo
The UCI team, lead by Cardiology Chair Dr. Pranav Patel, is astoundingly efficient and effective. Dr. Patel sent me through a journey of tests, heart monitoring, imaging and medications to rule out other causes of my situation. Rather than rush into surgery, he collected the data in order to make an informed decision as to the best course of action. Dr. Patel presented the information as the patient’s choice, with pros and cons for taking action. This solidified my confidence in the strategy – it was the right time to address the leak in my heart!
As a bike rider, I likened the original diagnosis, through an ultrasound test called a “bubble test” to the soap bubble on a tire tube. The solution was like getting a high-tech “bacon” plug on a tire.

The Gore Cardioform Septal Occluder
Procedure Day
First, registration at UCI was far and away the best experience I have had. Their caring staff explanied and resolved all issues, settling nerves for both me and my support people. They could give a tutorial to others regarding patient care and registration.
Second, getting prepped was done by talented nurses who worked efficiently and thought ahead, making the process smoother for the patient and surgical team.
The Anesthesiologist visit set the stage for expectations and process of my procedure, so there were no hanging questions and a good sense of the process for the procedure.
When it was time I was whisked Into the procedure room – the Cath Lab hybrid room. The team grew to a small but active crowd. Nurses, Anesthesiologist, Residents, Fellows, Device Reps, Surgeons. All had assignments as I drifted to sleep.
PFO Closure
The procedure was a balanced combination of expertise, medical technology and care. Dr Patel and his team brought the device in through the vein from my right leg, guided by ultrasound and fluoroscopy. The device fit through the PFO between right and left atria, and then opened on the left side. Pulling it back, the left side released into place. Then the moment of final release, as Dr. Patel put it: “Release the Kraken” as the right side popped open and the device was released like an inner space probe. Live ultrasound proved that the device was working.
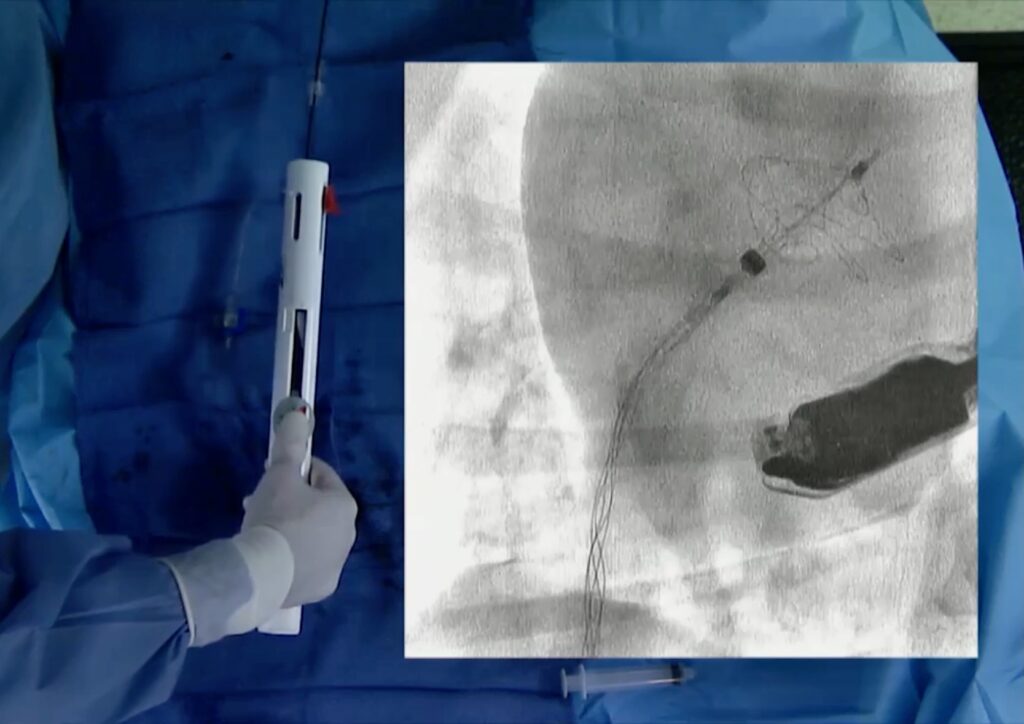
Gore Medical PFO closure device:
Recovery
The immediate recovery was smooth except for the noises and inconvenience of a long night in a busy hospital. I was not too rested the next day but felt well enough to walk, eat and leave. First a battery of tests including X-Ray and Ultrasound. And a visit with Dr. Patel, his Residents and Fellows, all eager to share the efforts and make sure the patient was safe and sent on his way.
Two weeks later, my follow-up appointment resulted in an all-clear. No signs of infection or complications and I was able to return to normal activity.
In October, a new ultrasound is the next step to observe the progress of my heart growing around the Gore Medical device. I have been told it will take 2 to 6 months to fully heal around the device
Final Thoughts
1.Listen to your body and get to the care you need. It may not be the biggest or closest, but seek out the best.
2. Talented health care teams will search for the right answer to your needs. Be patient and willing to give a lot of blood and take a lot of tests. Data is your friend.
3. The best care is top-to-bottom and involves . It’s pretty easy to see the nature of the culture of a location as a patient. Everyone should be on board and it will show.
4. The best care truly includes the patient (and any support caregivers). Beware if you feel you are being told instead of engaged.
5. Seek out and listen to those who have had a similar situation. Even if their condition may be different, you find quickly that you are not alone.



0 Comments